The human brain, a marvel of biological engineering, remains vulnerable to insidious processes that gradually erode its function. Among the most perplexing and devastating of these are neurodegenerative diseases, where the very building blocks of neurons – proteins – turn against the intricate machinery they once supported. At the heart of this betrayal lies a fundamental biological flaw: protein misfolding, a process where molecules crucial for cellular function twist into malignant shapes, triggering cascades of destruction.
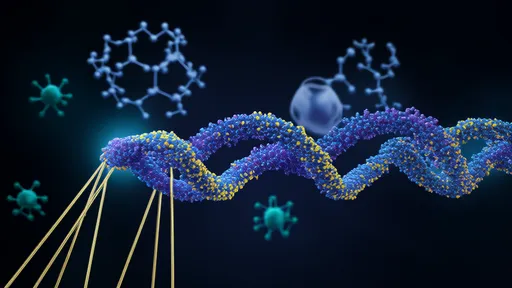
For decades, researchers have grappled with the paradox that proteins essential for life can morph into lethal agents. In Alzheimer's disease, amyloid-beta peptides clump into sticky plaques between neurons, while tau proteins form tangled fibrils inside cells. Parkinson's disease reveals a similar pattern, with alpha-synuclein aggregating into Lewy bodies that disrupt dopamine production. These pathological hallmarks aren't merely bystanders but active participants in neuronal demise, though the exact mechanisms remain hotly debated.
The protein folding problem extends far beyond simple structural errors. Cellular quality control systems, including chaperone proteins and the ubiquitin-proteasome pathway, typically identify and rectify misfolded molecules. However, when these systems become overwhelmed or dysfunctional, aberrant proteins accumulate. Some researchers propose that small, soluble oligomers – intermediate forms of misfolded proteins – may be more toxic than the large, insoluble aggregates visible under microscopes. These oligomers can perforate cell membranes, disrupt synaptic communication, and trigger inflammatory responses from microglia.
What makes certain proteins particularly prone to misfolding remains an area of intense investigation. Genetic mutations account for some cases, as seen in familial forms of neurodegenerative diseases. The APOE ε4 allele, for instance, dramatically increases Alzheimer's risk likely by influencing amyloid-beta clearance. Environmental factors also play significant roles – pesticide exposure has been linked to Parkinson's, while traumatic brain injury may accelerate tau pathology. Aging, the greatest risk factor for most neurodegenerative diseases, likely contributes through declining protein quality control mechanisms and cumulative cellular damage.
The spread of misfolded proteins through the brain follows disturbing patterns. Prion-like mechanisms, where malformed proteins induce normal counterparts to adopt pathological conformations, may explain the stereotypical progression seen in many diseases. In Alzheimer's, pathology often begins in memory-related regions before spreading diffusely. Parkinson's typically starts in the brainstem before affecting motor control areas. This propagation might occur through synaptic connections or extracellular spaces, with different proteins exhibiting distinct "strains" that influence disease characteristics.
Diagnostic challenges abound because symptoms often emerge only after substantial neuronal loss occurs. Biomarkers like cerebrospinal fluid protein levels and PET imaging of amyloid or tau provide windows into disease processes, but accessibility remains limited. Blood-based biomarkers showing promise could revolutionize early detection, allowing interventions before irreversible damage accumulates. The recent development of alpha-synuclein seed amplification assays for Parkinson's exemplifies this progress, detecting pathological forms years before symptom onset.
Treatment strategies have evolved from symptom management to targeting root causes. Monoclonal antibodies like aducanumab and lecanemab, which clear amyloid-beta, represent first-generation disease-modifying therapies for Alzheimer's, albeit with modest clinical benefits. Small molecules that inhibit protein aggregation or enhance clearance mechanisms show potential in preclinical studies. Gene therapies aiming to silence mutant genes or boost protective factors are entering clinical trials. Perhaps most intriguing are approaches targeting protein folding itself – pharmacological chaperones that stabilize native conformations or compounds that redirect misfolded proteins toward degradation pathways.
The complexity of neurodegenerative diseases demands equally sophisticated research models. Traditional cell cultures and animal models, while invaluable, often fail to fully recapitulate human pathology. Human induced pluripotent stem cell-derived neurons now allow study of patient-specific disease mechanisms. Organoids – miniature, simplified versions of brain structures – enable observation of protein pathology in three-dimensional environments. Computational models predicting protein folding dynamics and artificial intelligence analyzing vast datasets are accelerating discovery in ways unimaginable a decade ago.
Beyond medical interventions, lifestyle factors influence protein homeostasis. Exercise enhances cellular stress responses and protein quality control. Dietary patterns like the Mediterranean diet may reduce inflammation linked to protein misfolding. Cognitive engagement appears to build resilience against pathology, the concept of cognitive reserve. While these measures don't prevent disease outright, they may delay onset or slow progression, buying valuable time for developing more effective treatments.
The socioeconomic burden of protein misfolding disorders grows as populations age, with costs extending far beyond healthcare to lost productivity and caregiver strain. This crisis spurs unprecedented collaboration between academia, industry, and patient advocacy groups. Open science initiatives share data across institutions, while adaptive clinical trial designs accelerate therapeutic evaluation. Patient registries and biomarker studies create frameworks for precision medicine approaches tailored to individual disease subtypes.
Ethical considerations loom large as diagnostic capabilities outpace treatment options. The ability to predict diseases decades before symptoms raises questions about psychological impacts and insurance discrimination. Experimental therapies carry risks of serious side effects, as seen with brain swelling and microbleeds from amyloid-targeting antibodies. Equitable access to emerging treatments presents another challenge, with costly therapies potentially exacerbating healthcare disparities.
Looking forward, the protein misfolding paradigm continues to evolve. Once viewed as distinct entities, neurodegenerative diseases increasingly appear as spectra with overlapping mechanisms. The same proteins misfold in different ways to produce varied clinical pictures. This realization fuels search for common therapeutic targets that might benefit multiple conditions. Meanwhile, emerging research explores how protein misfolding interacts with other aging-related processes like mitochondrial dysfunction and neuroinflammation.
The journey from fundamental discoveries about protein structure to effective therapies has been longer and more arduous than anticipated. Yet each failed clinical trial yields insights refining subsequent approaches. As understanding of protein misfolding deepens, so does the potential to develop interventions that not just alleviate symptoms but halt or prevent the underlying disease processes. For millions affected by these devastating conditions and their families, this scientific pursuit represents hope against previously inexorable decline.

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 20, 2025

By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025